

Vaccine Details
Influenza vaccine
a. Age-wise Data of Infection and Deaths
Influenza impacts various age groups differently. During the 2022–2023 flu season in the United States, the Centers for Disease Control and Prevention (CDC) reported approximately 21,401 influenza-related deaths. Notably, individuals aged 65 and older accounted for about 15,399 of these deaths, indicating a mortality rate of approximately 26.6 per 100,000 in this age group. In contrast, the mortality rate among those aged 18 to 49 was about 0.7 per 100,000.b. Impact of Vaccination on Reducing Morbidity and Mortality
Influenza vaccination plays a significant role in reducing illness and death: Reduction in Mortality: Vaccination of healthcare workers has been associated with a substantial decrease in mortality among patients, particularly in long-term care settings. Decreased Hospitalizations: Studies have shown that influenza vaccination reduces the incidence of severe respiratory infections, thereby decreasing hospital admissions.c. Staff Leave and Productivity in India
Influenza significantly affects workplace productivity due to increased absenteeism. The World Health Organization (WHO) notes that influenza epidemics can lead to high levels of worker absenteeism and productivity losses Vaccination of healthcare personnel has been shown to reduce staff illness and absenteeism, thereby maintaining a more stable workforced. Family Transmission of Office-Acquired Infections
Infections contracted in the workplace can extend to household members: Household Spread: Employees infected with influenza can transmit the virus to family members, leading to broader community outbreaks. Preventive Measures: Encouraging vaccination among employees not only protects the individual but also reduces the risk of transmitting the virus to family members, thereby safeguarding public health. (290,000 to 650,000 respiratory deaths worldwide)HPV Vaccine
Human Papillomavirus (HPV) vaccination plays a crucial role in reducing infection rates and associated cancer incidences across different age groups. Here's an overview addressing your points:
a. Age-wise Infection and Cancer Rates
HPV Infection Rates by Age: HPV is highly prevalent among sexually active individuals. In the United States, the prevalence among women aged 20 to 24 is approximately 44.8%, with rates decreasing in older age groups. Cervical Cancer Incidence by Age: Cervical cancer rates rise sharply from ages 15- 19, peaking in the 30-34 age group, then decline in older women.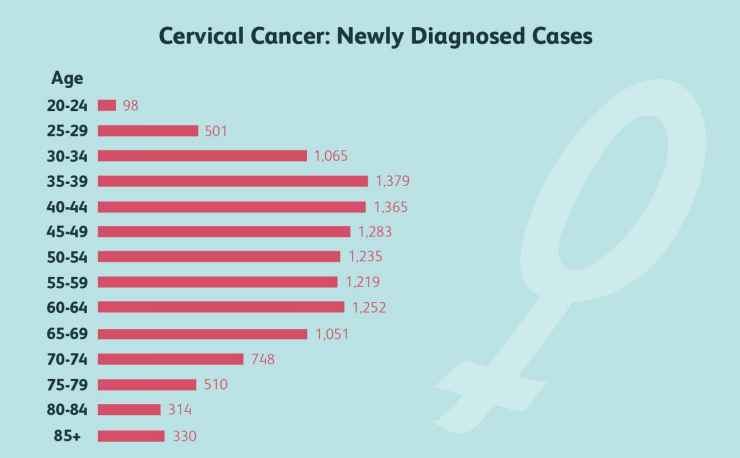
b. Impact of Vaccination on Cancer Rates
Reduction in Cervical Cancer Rates: Studies have demonstrated a substantial decline in cervical cancer incidence among vaccinated populations. For instance, in England, there was a significant reduction in cervical cancer and CIN3 (a severe cervical pre-cancer) in young women following the introduction of the HPV immunization program. Target Audience: Emphasize the importance of vaccinating young adults, particularly before they become sexually active, to maximize the vaccine's protective benefits. Engaging both young individuals and their parents is crucial to increase vaccination uptake.Studies have demonstrated a significant decline in cervical cancer rates among vaccinated populations. For instance, in England, there was a substantial reduction in cervical cancer and CIN3 (a severe cervical pre-cancer) in young women following the introduction of the HPV immunization program. Targeting young adults and their parents with this information can emphasize the vaccine's effectiveness. India reports approximately 1,23,907 new cervical cancer cases annually, with a crude incidence rate of 18.7 per 1,00,000 women. Certain states exhibit high rates of cervical cancer. Notably, Mizoram, Arunachal Pradesh, Karnataka, and Nagaland have Disability-Adjusted Life Years (DALYs) exceeding 300 per 100,000 women, indicating a substantial impact on health and productivity. In Arunachal Pradesh, Papum Pare district records the highest incidence rate of cervical cancer in Asia, at 27.7 per 100,000 women. These elevated rates may be attributed to factors such as limited access to healthcare, low awareness about HPV and its link to cervical cancer, and insufficient screening and vaccination programs. To combat this, the Indian government has initiated measures to introduce the HPV vaccine into the Universal Immunization Programme (UIP), targeting girls aged 9–14 years. This strategy aims to reduce the incidence of HPV-related cancers through proactive immunization efforts.(630,000 new cancer cases and approximately 311,000 deaths globally each year.)
Pneumococcus vaccine
a. Targeting Special Groups and Senior Citizens
Age-Based Recommendations: The Centers for Disease Control and Prevention (CDC) recommend pneumococcal vaccination for all adults aged 50 years and older.
High-Risk Populations: Individuals aged 19 to 49 with certain chronic conditions—such as chronic heart, lung, or liver diseases, diabetes, or weakened immune systems—are also advised to receive the vaccine due to their increased susceptibility to pneumococcal disease.
b. Hospitalization Costs and Mortality Rates
Reduction in Hospitalizations: Pneumococcal vaccination has been associated with a significant decrease in hospital admissions for pneumonia. A study reported a 43% reduction in pneumonia-related hospitalizations among vaccinated individuals.
Cost Savings: By preventing severe pneumococcal infections, vaccination reduces healthcare expenditures. Research indicates that vaccinated patients had shorter hospital stays and lower hospitalization costs compared to unvaccinated patients.
Decreased Mortality Rates: The same study observed a 29% reduction in mortality among vaccinated individuals, highlighting the vaccine's role in saving lives.
(approximately 1,189,937 deaths worldwide, with 341,029 of these occurring in children under five years old and 494,340 in adults over 70.)Herpes zoster vaccine
Importance of Addressing Pain from Recurrent Lesions
Shingles manifests as a painful, blistering rash that typically appears on one side of the body. The pain can be severe and debilitating, often described as burning, stabbing, or gnawing. In some cases, even after the rash resolves, individuals may experience postherpetic neuralgia (PHN), a chronic nerve pain that can persist for months or even years.
Chickenpox Rates in India and Latent Infection
In India, chickenpox remains a common childhood disease, with most individuals acquiring the infection by adulthood. The varicella-zoster virus, after causing the initial chickenpox infection, becomes latent in the body's nerve tissues. This dormant virus can reactivate later in life, especially when the immune system is weakened due to factors like aging, stress, or immunosuppressive conditions, leading to shingles. The prevalence of chickenpox in the population thus establishes a reservoir for potential herpes zoster cases in the future. Implementing widespread varicella vaccination can reduce the incidence of primary infections, thereby decreasing the pool of individuals at risk for shingles later in life.
Potential Link Between Herpes Zoster and Alzheimer's Disease
Emerging research suggests a possible association between VZV reactivation and an increased risk of neurodegenerative conditions, including Alzheimer's disease. A study published in the Journal of Alzheimer's Disease indicated that VZV reactivation might lead to neuroinflammation, potentially accelerating the progression of Alzheimer's. The proposed mechanism involves VZV-induced inflammation triggering the reactivation of latent herpes simplex virus type 1 (HSV-1) in the brain, which has been implicated in Alzheimer's pathology. While these findings are preliminary, they highlight the importance of preventing VZV reactivation through vaccination, not only to avert shingles and its immediate complications but also to potentially reduce the risk of long-term neurological sequelae.
(equating to approximately 0.28–0.69 deaths per 1 million population.)Measles Mumps Rubella vaccine
a. Targeting Parents of Unvaccinated Young Children
Recent outbreaks underscore the critical need for MMR vaccination. In West Texas, a measles outbreak resulted in 124 cases across nine counties, predominantly affecting unvaccinated school-aged children. Tragically, this led to the first measles-related death in the U.S. since 2015—a school-aged child who had not received the MMR vaccine. Measles is highly contagious; up to 90% of unvaccinated individuals exposed to the virus will become infected. Complications can be severe, including pneumonia, encephalitis, and death. The MMR vaccine is approximately 97% effective in preventing measles and also offers protection against mumps and rubella. Ensuring children receive the MMR vaccine not only safeguards their health but also contributes to community immunity, protecting those who cannot be vaccinated.
b. Mumps Orchitis in Males and Potential Fertility Implications
Mumps, another component of the MMR vaccine, can lead to orchitis—inflammation of one or both testicles—in post-pubertal males. This condition occurs in approximately 40% of males who contract mumps after puberty. While unilateral orchitis (affecting one testicle) often resolves without long-term effects, bilateral orchitis (affecting both testicles) can lead to testicular atrophy and has been associated with infertility or subfertility in 30% to 87% of cases. Preventing mumps through MMR vaccination is crucial to avoid these severe complications. Parents should be informed that vaccinating their children not only protects against immediate illness but also preserves future fertility in males. The MMR vaccine is safe and effective, with the benefits far outweighing the minimal risks associated with vaccination.
(approximately 107,500 deaths, predominantly among children under five years of age.)Hepatitis B vaccine
Emigrant College StudentsEmigrant college students, especially those from regions with high hepatitis B virus (HBV) prevalence, may be at increased risk of HBV infection. The Centers for Disease Control and Prevention (CDC) recommend that all adults aged 18 and older be screened for HBV at least once in their lifetime Vaccination is strongly advised for those who are not immune, as it provides effective protection against HBV infection.
Antibody Screening and Vaccine EfficacyPost-vaccination antibody screening is essential to confirm immunity, particularly in high-risk groups. An anti-HBs (hepatitis B surface antibody) level of ≥10 mIU/mL indicates adequate protection. Studies have shown that immune memory against HBV can last for at least 30 years post-vaccination, even if antibody levels decline below detectable levels However, certain populations, such as those undergoing hemodialysis, may exhibit a reduced response to the vaccine. In these cases, a higher vaccine dose or additional booster doses may be necessary to achieve adequate immunity.
Risk in Families with Members Undergoing DialysisIndividuals on hemodialysis are at an increased risk of HBV infection due to potential exposure during treatment. Family members of dialysis patients may also be at risk, as HBV can be transmitted through close personal contact. Vaccination of both patients and their household contacts is crucial to prevent transmission. Research indicates that hepatitis B vaccination significantly reduces the risk of acquiring HBV infection in chronic hemodialysis patients
Hepatitis A Vaccine in Outbreak Situations Hepatitis A is a highly contagious liver infection, often transmitted through contaminated food or water. In outbreak scenarios, vaccination is a key control measure. The World Health Organization (WHO) recommends hepatitis A vaccination for individuals at increased risk of infection, including those in outbreak settings Cholera and Enteric Fever Vaccination Cholera and enteric fever (typhoid) are severe gastrointestinal diseases prevalent in areas with inadequate sanitation. During outbreaks, vaccination serves as an effective preventive strategy. The WHO emphasizes the importance of cholera vaccination in outbreak settings to control the spread of the disease. Similarly, typhoid vaccination is recommended, especially for travelers to regions where the disease is endemic. (estimated 1.1 million deaths globally)Gulbarga, Karnataka:
A study conducted in Gulbarga highlighted a 7.11% seroprevalence of HBV among individuals frequenting local barbershops. This elevated rate is attributed to practices such as the reuse of razors and inadequate sterilization, which facilitate HBV transmission.
Andhra Pradesh:In Andhra Pradesh, certain communities exhibit higher HBV prevalence. For instance, the Lambada tribal population has an HBsAg positivity rate of 5.16%
Maintaining Vaccination Health Records & Issuing Certificates for Travel, Emigration, and Medical Documentation:
How We Maintain Health Records:- ✅ Digital Vaccination Records: Each vaccination is logged into a secure digital database for easy access.
- ✅ Personalized Vaccination History: Providing individuals with a consolidated record of all administered vaccines.
- ✅ Automated Reminders & Updates: System sends timely alerts for upcoming booster doses, ensuring continued protection.
- ✅ Travel & Emigration Compliance: Government-approved and WHO-compliant certificates required for international travel and visa applications.
- ✅ QR-Code Verified Digital Certificates: Secure, tamper-proof certificates accessible via mobile or email.
- ✅ Hard Copy Issuance: Printed vaccination records for submission at embassies, workplaces, or health authorities.
- ✅ Compliance with IHR (International Health Regulations): Ensuring records are recognized globally.
- ✅ Linkage to Government Portals: Where applicable, integrating with official health registries for authenticity.
NOTE:Besides the key vaccines listed above, we offer a comprehensive range of vaccinations tailored to individual needs and medical requirements. Our experts will guide you through the process by asking a few simple questions, helping you determine the most suitable vaccinations for your health and well-being.